Informed consent is a process SLPs need to be aware of when working with patients. Obtaining informed consent is the responsibility of the healthcare provider who is making the recommendations. How is informed consent obtained by SLPs?
- Utilize shared decision-making for your patients. Shared decision-making includes patient-centered conversation and ensuring decisions utilize the best evidence paired with the person’s values and preferences.
- Imaging can support best evidence and reduce defensive practices in dysphagia management.
- Informed consent is a continuing process that occurs over multiple sessions and may involve multiple care team members.
- Documentation of the conversations is an imperative part of the process. “In shared decision-making with the patient…”
Ensuring that patients are prepared to engage in these conversations supports the informed consent process. The SPIKES method can be used as a structured communication framework for both obtaining informed consent and fostering genuine shared decision-making in patient care.
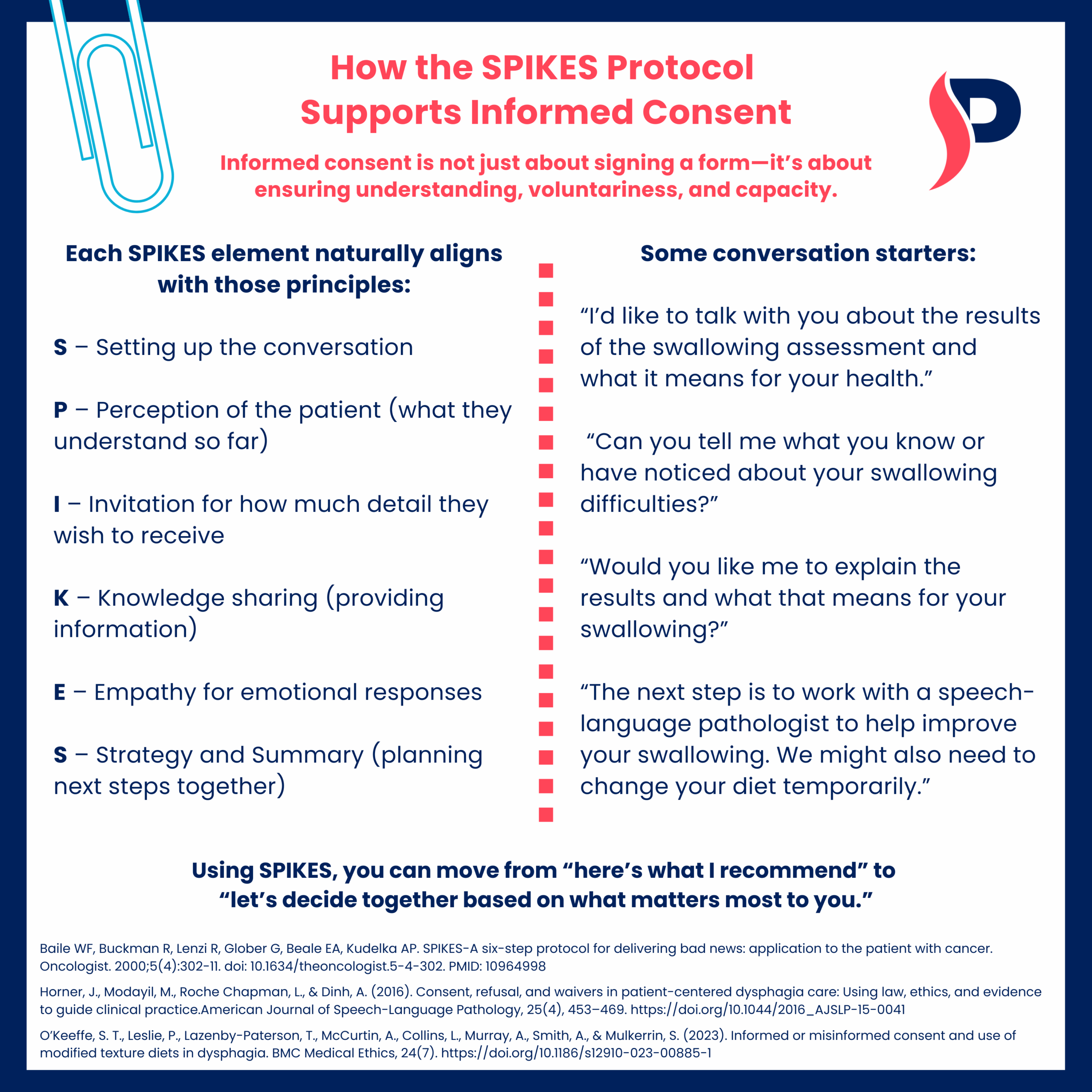
How the SPIKES Protocol Supports Informed Consent
Informed consent is not just about signing a form—it’s about ensuring understanding, voluntariness, and capacity.
Each SPIKES element naturally aligns with those principles:
S – Setting up the conversation
P – Perception of the patient (what they understand so far)
I – Invitation for how much detail they wish to receive
K – Knowledge sharing (providing information)
E – Empathy for emotional responses
S – Strategy and Summary (planning next steps together)
Some conversation starters:
“I’d like to talk with you about the results of the swallowing assessment and what it means for your health.”
“Can you tell me what you know or have noticed about your swallowing difficulties?”
“Would you like me to explain the results and what that means for your swallowing?”
“The next step is to work with a speech-language pathologist to help improve your swallowing. We might also need to change your diet temporarily.”
Using SPIKES, you can move from “here’s what I recommend” to “let’s decide together based on what matters most to you.”
Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302-11. doi: 10.1634/theoncologist.5-4-302. PMID: 10964998
Horner, J., Modayil, M., Roche Chapman, L., & Dinh, A. (2016). Consent, refusal, and waivers in patient-centered dysphagia care: Using law, ethics, and evidence to guide clinical practice.American Journal of Speech-Language Pathology, 25(4), 453–469. https://doi.org/10.1044/2016_AJSLP-15-0041
O’Keeffe, S. T., Leslie, P., Lazenby-Paterson, T., McCurtin, A., Collins, L., Murray, A., Smith, A., & Mulkerrin, S. (2023). Informed or misinformed consent and use of modified texture diets in dysphagia. BMC Medical Ethics, 24(7). https://doi.org/10.1186/s12910-023-00885-1
DOWNLOAD THESE CLINICAL CLIPS
DOWNLOAD CLIP 1 HERE + DOWNLOAD CLIP 2 HERE